Medical professionals lead a tough life in every aspect, from facing severe traumatic cases to witnessing the infinite pain and suffering in the eyes of the patient's families to the tremendous hectic schedule they face day-in and day-out. Considering this scenario, mental and physical exhaustion is very much legitimate. Especially in the pandemic and post-pandemic era, the situation worsened among professionals. Burn-out is seen to be very commonly witnessed among medical professionals since the beginning. In recent times considering the COVID-19 pandemic, medical professionals are very much facing episodes of burnout. Burnout can have serious consequences for both patients and healthcare professionals. This leads to poor physical and mental health outcomes, lack of motivation, and poor staff morale, and poor quality of care provided by affected staff. As a result, the patient's results are reduced. Several systematic reviews have found that high levels of burnout among medical professionals are associated with unsafe patient care.
The deadly and uncontrollable nature of COVID-19, combined with the relatively high infection and mortality rates of HCP, can cause anxiety and stress among healthcare professionals. Problems such as social stigma, lack of personal protective equipment, and hard work of staff can exacerbate this situation. Therefore, this pandemic is expected to have a significant psychological impact on healthcare professionals (HCPs). Frontline healthcare professionals involved in the treatment and diagnosis of COVID-19 are faced with greater overwhelming pressure with the resulting psychological stress. Due to ethical dilemmas and moral wounds, healthcare professionals must be quickly guided to the pain of life and death decisions without the support of optimal care protocols.
Our DBMR team has analyzed and investigated the COVID-19 infection market and witnessed that lack of awareness and safety among people and increasing investment for healthcare infrastructure are the major drivers boosting market growth. It had a CAGR of 12.80% during the forecast period of 2022 to 2029.
To know more about the study, kindly visit: https://www.databridgemarketresearch.com/reports/global-covid-19-infection-market
Prevalence
- According to 2020 National Physician Burnout and Suicide Report Medscape report, it was witnessed that a burnout rate of about 43% was seen in 2020, which remains quite similar to the 46% reported in 2015 and 39.8% in 2013
- According to the study "Burnout among healthcare providers in the complex environment of the Middle East" conducted by Z.Chemali, among physicians undergoing residency program in the UAE (N = 302), about 70% of participants reported general burnout, 84% reported severe depersonalization, 75.5% reported moderate to severe emotional malaise, and 74% reported a diminished personal sense of accomplishment. Among Iranian emergency physicians (N = 85), participants' burnout levels at three subscales of emotional fatigue, depersonalization, and perceived decline in performance were 84.5% and 48.1, respectively. It was high at%, and 80.5%.
- According to the study titled, "Burnout among healthcare professionals during COVID-19 pandemic," conducted by Mohammad Jalili et.al, healthcare workers from six university-affiliated hospitals who had been taking care of COVID-19 patients were studied. It was found that 326 (53.0%) experienced high levels of burnout. The average scores for emotional fatigue, depersonalization, and lack of personal achievement were 26.6, 10.2, and 27.3, respectively. The degree of burnout in the three subscales varied based on personal and work-related factors, and gender was the only variable associated with high scores in all three domains.
- The reported incidence of burnout varies worldwide. For instance, there are differences between countries within the European Union (10%) and countries outside the European Union (17%). In European Union countries, burnout ranges from 4.3% in Finland to 20.6% in Slovenia and 13% in Albania to 25% in Turkey in non-European countries22. Actively related to workloads.
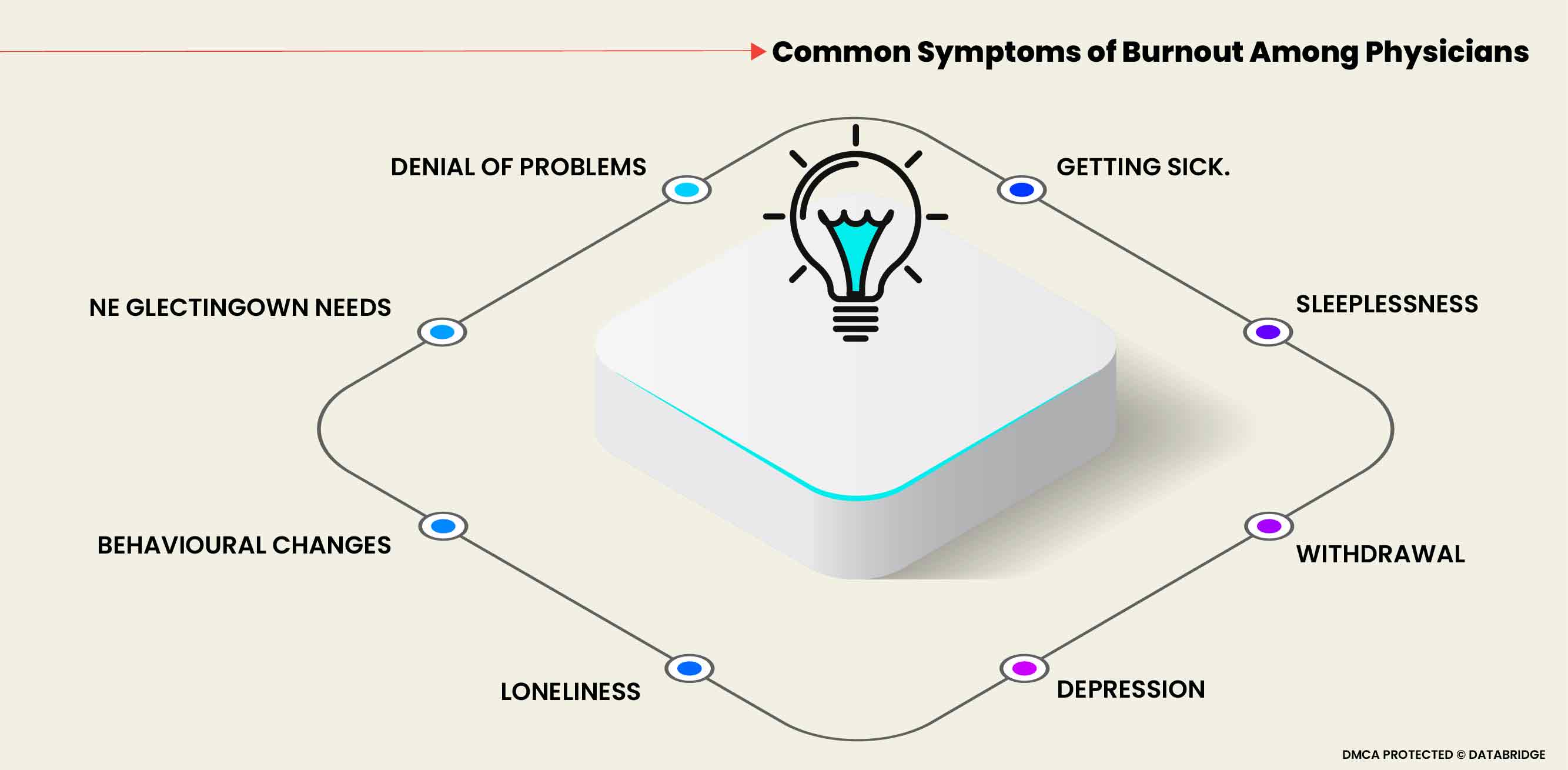
What Are The Symptoms Associated With Burnout?
The common symptoms associated with the burnout phenomenon among medical professionals are: Denial of problems, neglecting own needs, behavioral changes, loneliness, depression, withdrawal, sleeplessness, and getting sick.
The symptoms associated with burnout syndrome are very elaborative and well explained in the following section. This is a 5-stage model starting with the honeymoon phase, then with the onset of stress, chronic stress, and burnout, and ending with habitual burnout.
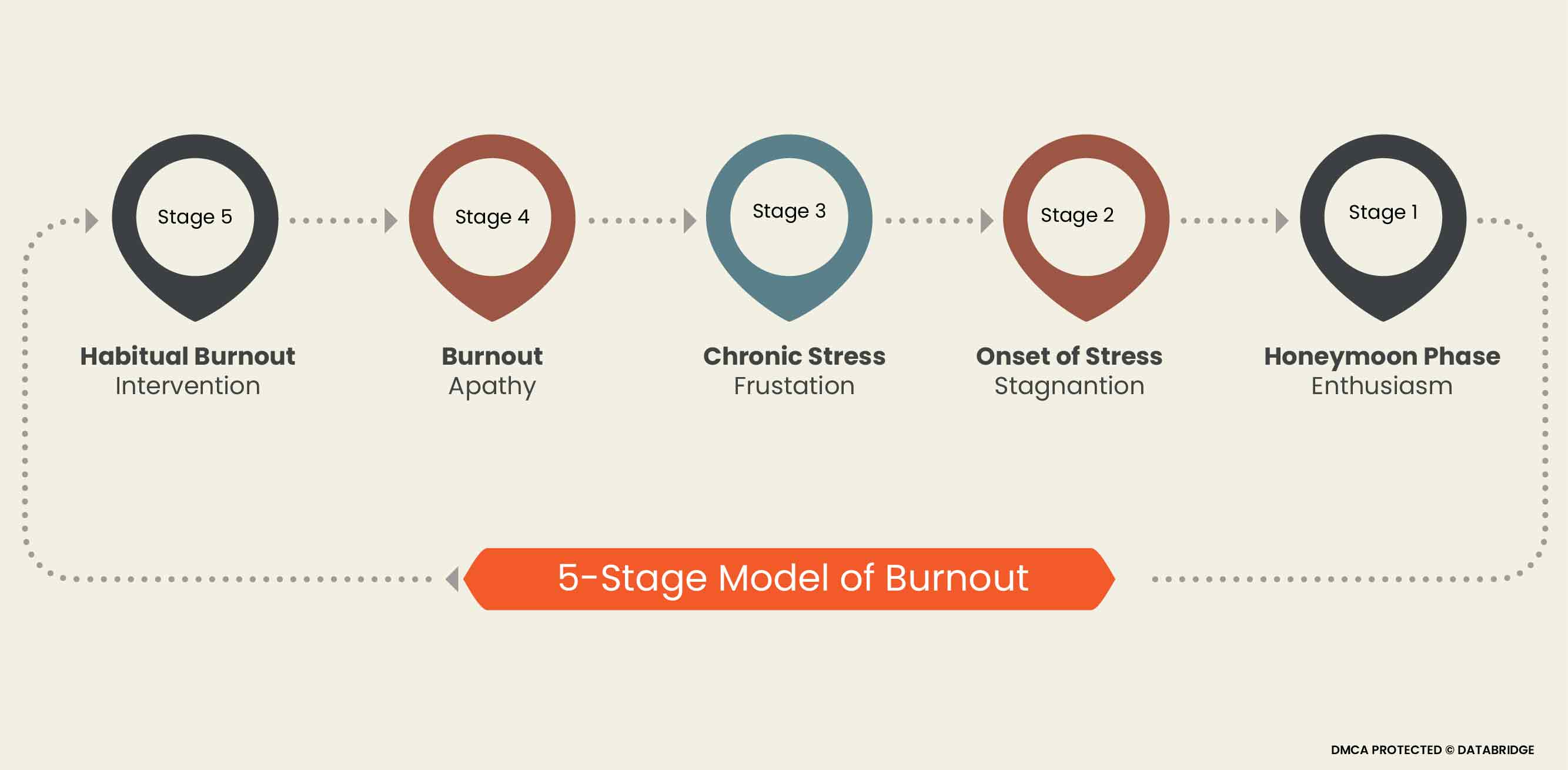
This 5-step model begins in the honeymoon phase and features enthusiasm. But over time, this inevitably becomes associated with experiencing work stress. Burnout can begin if no aggressive coping strategy is implemented at this stage. This is followed by a period of stagnation characterized by the onset of stress. This second stage begins with recognizing that one day is more complex than another. Life is limited to work and business, family, social life and personal priorities are ignored, symptoms of suffering and stress are frequent, and emotionally and physically affected. After that, a stage of chronic stress develops, leading to frustration. Individuals get a sense of failure and helplessness. Efforts are not visibly rewarded, and the perceptions and facts of not getting enough credit make us feel incompetent and inadequate. Then this leads to a stage of indifference, where despair and disillusionment occur. People can't see how to get out of the situation, resign, and become indifferent. The final stage is habitual burnout. Burnout can cause serious physical or emotional problems, ultimately leading to seeking help or intervention. The list of symptoms is long; most are not very specific. Symptoms are associated with different stages of the syndrome and are divided into different clusters. These include early warning symptoms (increased commitment to goals and malaise) followed by a phase of decreased commitment (to patients and, clients, others). Emotional reactions and accusations (depression, aggression) ultimately lead to cognitive ability, motivation, creativity, impaired judgment, and emotional. It leads to flattening of social and intellectual life, psychosomatic reaction, and despair.
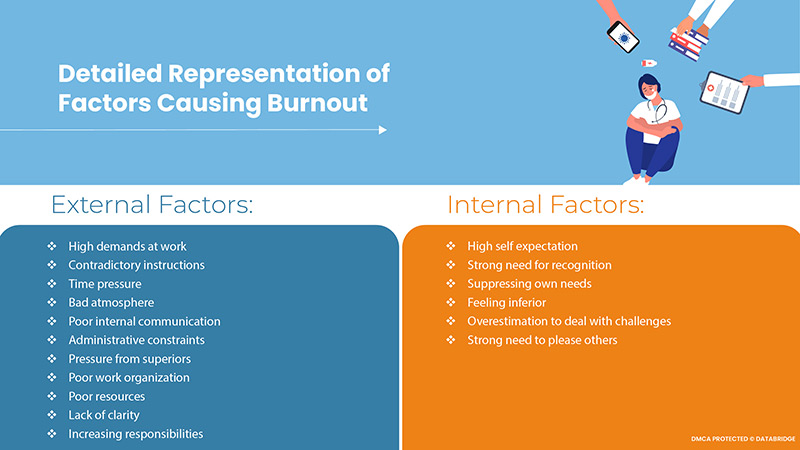
What are the Factors Leading to Burnout?
Although it seems to be a very broad term, several factors lead to burnout among medical professionals. These factors were considered in developing various psychological explanatory models for the etiology of burnout. Several external factors accelerate the situation, and many internal factors also lead to the development of the same.
Dependence of Strain on Healthcare Jobs
The stress level represents a requirement in the workplace that can cause stress. This includes workload, including work pace, availability, time pressure, travel time, and task difficulty. The scope of decision-making refers to the ability and freedom of employees to organize and manage their workloads. Based on these concepts, diagrams representing four different work situations have been proposed, taking into account both the stress caused by the work situation and the personal attitudes and commitments of the employees. These are low-load and high-load jobs, and passive and active jobs. The stress-free work represents a combination of work that does not have significant demanding tasks but has an agency such as employees' freedom to set their schedules and goals. This section represents most of your daily work. People in this category can become increasingly bored with their work situation.
In contrast, high-stress work refers to highly demanding and complex work with little employee control over working conditions and goals. The risk of stress increases accordingly. Passive jobs are simple jobs, but they have little decision-making power and are usually repetitive production jobs. Such work does not mean much stress, but it is not a big challenge for employees either. On the other hand, active work is very demanding, and employees have plenty of room for decision making.
The consequences of burnout are reduced work satisfaction, absenteeism, staff turnover, and cynicism. These work impacts often have the following personal impacts: Unhappiness, anxiety, depression, isolation, substance abuse, friction, disruption of relationships, and feelings of divorce. Physician burnout can have a more serious professional impact than in other professions. In fact, physician burnout is associated with poor patient care, resulting in poor patient satisfaction and poor quality of care. This can ultimately lead to malpractice, which can lead to malpractice allegations and subsequent litigation, resulting in high costs for caregivers and hospitals.
What is the Direct Consequence of Burnout on Healthcare Workers?
Of course, the first direct impact of burnout lies in the care and safety of the health care workers themselves. Depression rates in health care workers are alarming compared to the general population and are closely associated with high levels of work-related stress. A meta-analysis investigating the mental health of health care workers during the outbreak of COVID-19 reported a relatively high prevalence of anxiety (24.94%), depression (24.83%), and sleep disorders (44.03%). (23, 24). Healthcare professionals tend to hide their difficulties because of the perceived stigma surrounding mental illness and the fear of career implications.
Our DBMR team investigated the anxiety disorder market and witnessed the rising prevalence of personality disorders and stress build-up, especially in adults, rising awareness programs worldwide through campaigns & media and an increased female adult population. In addition to this, North America dominates the market share due to increased investment by pharmaceutical industries for the advancement in the treatment and favorable reimbursement scenario.
For know more about the study, kindly visit: https://www.databridgemarketresearch.com/reports/global-anxiety-disorder-market
These mental states are associated with other criticisms, including a 25% increase in the likelihood of alcohol abuse or addiction and a double risk of suicidal ideation. At the extreme, doctors are known to have a higher rate than the general public. Many reports show a standardized all-cause mortality rate for physician suicide, with a high female value of 1.99. They also found high risk for anesthesiologists, psychiatrists, general practitioners, and general surgeons. A data set on the effects of COVID-19 on doctors' mental health and suicide is currently unavailable, but the massive news published in various national newspapers about the suicides of doctors working in a pandemic is if it gets worse. The indirect effects of burnout can be poor quality of the medical system in terms of compliance, lack of communication, malpractice, patient outcomes and safety. Medical professionals suffering from burnout may not be able to provide quality medical services, take unnecessary risks, and pay attention to details. Awareness of exposure to adverse events or poor quality of care can lead to psychological distress. Appropriate measures need to be taken to take care of these changes and implement measures according to the severity.
Effect of Burnout on Nurses
The burnout syndrome leaves much impact on the nurses as well. Numerous research has shown how detrimental burnout is. Nurses' quality of life, level of performance, and organizational commitment are all negatively impacted by burnout, which also increases their intention to quit. Burnout also raises turnover rates and degrades the standard of nursing care. Organizational traits and leadership behaviors that enable nurses to take charge of their work by using their knowledge, actions, and abilities can enhance organizational commitment, job satisfaction, and care quality. They can also boost management confidence and lessen nurse burnout. When viewed through the lens of the features of the professional practice environment, structural empowerment was found to be significant for nurses' job satisfaction as well as the standard of patient care. Additionally, it was shown that empowerment on both a structural and psychological level were critical for reducing burnout and increasing intent to stay.
Through the facilitation of trust in the leader and organization, an empowering leadership style (setting an example, imparting knowledge, and demonstrating concern for the team) lowers nurses' experiences of emotional tiredness and depersonalization. Increases in age and nursing experience are positively correlated with high levels of burnout as measured by high levels of emotional empowerment; this association may be explained by the rise in personal and professional duties that comes along with age and experience. However, many studies revealed that personal accomplishment is also favourably correlated with age and experience, which may be related to rises in nurses' satisfaction with their job contribution. Redesigning a work schedule to give older and more seasoned nurses regular short-term breaks during their shifts, do voluntary overtime, reduce workload, and increase control over their practice is necessary since as time passes, their self-esteem and self-efficacy in performance both increase, and they become more susceptible to emotional empowerment.
The most crucial factor in emotional empowerment is the type of hospital, suggesting that the nurse's work environment may play an important role in the nurse's burnout emotions. In addition, the two leader empowering behaviors were the factors that influenced emotional empowerment. It is about providing autonomy and facilitating opportunities to participate in decision-making. This suggests that caregivers lack of autonomy and practice control can cause burnout. Concerning depersonalization, three factors have proved to be influential: gender, promotion of decision-making opportunities, and department type. In fact, by being involved in work-related decisions, nurses find it important to contribute to work and improve their attitude towards patients. In addition, two factors predicted personal accomplishment. It is a leader's role to facilitate goal achievement and nursing experience. Achieving organizational goals is important for caring for personal accomplishment, as personal accomplishment provides evidence of success at work, and this sensation is enhanced by increased experience.
How to Deal With These Situation?
Approaches for treating burnout should be based on the severity of the symptoms. If these are small and minor, measures such as lifestyle changes and optimizing the balance between work and life are recommended. These measures focus on three key pillars: stress relief, relaxation, and sports recovery.
As Michael Gungor rightly said, 'Burnout is what happens when you try to avoid being human for too long'.
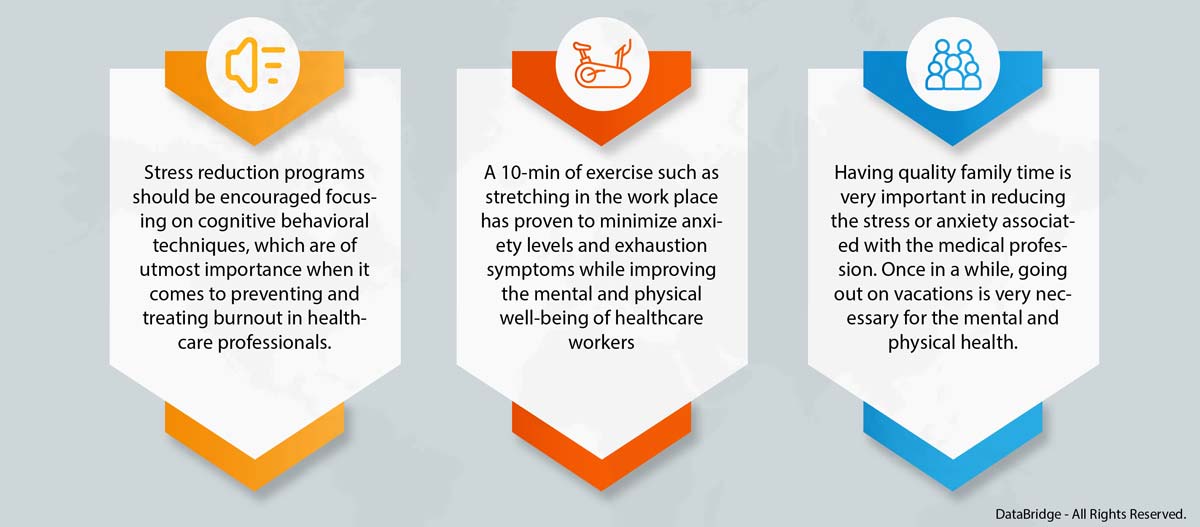
Besides these key pillars, there are other interventions that will help manage the burnout release among healthcare professionals.
- Recognizing burnout is the first step in finding a solution. You can start a peer-to-peer coaching session at the department level. In this session, teachers, residents and trainees will have the opportunity to seek advice from colleagues and mental health professionals on how to express their feelings, manage burnout and promote welfare permits.
If you complain, you are not considered resilient. This idea is harmful and can lead to despair and self-judgment. How can we be considerate of our patients when we are very critical of ourselves? By deepening bonds through shared experiences, peer-to-peer coaching can help someone experience a feeling of loneliness or isolation. This strategy can also eliminate the general hierarchy in medicine, especially in the surgical field.
- The next step is to have a list of outreach programs and anonymous psychological health support contact information on each department's website's Mental Health Resources page.
According to a recent Medscape report, nearly 40% of US doctors did not receive workplace support to deal with grief and trauma. Healthcare workers work overtime, and some feel that they do not have time or are safe to discuss their emotional and mental health with their colleagues. Anonymous ways to access mental health resources are important to them.
- Program directors, associate program directors, and faculty should be provided with empathic supervision training to facilitate an open discussion with medical students, residents, and fellows on burnout and well-being. Trainees deserve full attention to their emotional and mental health, even for just a few minutes.
Dialogues such as "Tell me, how do you really get over this pandemic?" helps a lot. Providing a safe space for trainees by actively listening and acting is the most important thing we can do as mentors.
Our DBMR team investigated the mental health and substance abuse services market and witnessed that new innovations in healthcare and rise in the prevalence of mental health disorders are the major drivers in this market. Asia-Pacific is expected to register the highest CAGR from 2021 to 2030 due to increased health awareness, improved healthcare infrastructure, and an increase in the number of hospitals with modern medical facilities.
To know more about the study, kindly visit: https://www.databridgemarketresearch.com/reports/global-mental-health-and-substance-abuse-services-market
- Organizational leadership must implement a comprehensive action plan to promote well-being and prevent burnout. This may require a cultural shift from treating acute mental health problems to promoting programs to improve physician well-being and resilience. In 2019, the American Medical Association launched the Joy in Medicine certification program. The program encourages organizational leaders to improve physician well-being and reduce burnout by making workplace changes that will enhance practice efficiency, teamwork, and health care.
- Hospital managers should establish a multi-department provider wellness committee that includes physicians and advanced care providers. Each department may have a "wellness champion" who can discuss department-specific issues, but it can also be a wellness window for other faculties and residents within the department. Hospitals can work with the provider's wellness committee to prioritize spaces for wellness-related conversations. If these small changes make sense and improve the well-being of healthcare professionals, hospitals should consider creating an environment without electronics. Federal, state, and city governments need to support such programs and encourage research to optimize the welfare of health care workers. Such collaboration could even advance the science of burnout during this pandemic.
How Can Nurses Prevent Burnout?
How to prevent a nurse's burnout? Fortunately, it's possible to avoid a nurse's burnout before it happens — and treat it as soon as it happens. For healthcare institutions, preventing nurse burnout protects staff, patients, and profits. Nursing managers and supervisors can help prevent burnout and reduce workplace risk. And the caregiver himself can take preventive and therapeutic measures for self-care.
- Coping Methods- One of the best ways to manage your work stressors is to learn coping skills. Methods such as breathing techniques, restorative exercise, journaling, and a post-work relaxation routine can make a big difference in your physical and mental health and well-being as a healthcare worker.
- Schedule Improvement- Nurse managers should schedule staff humanely with shift lengths of up to 9 hours whenever possible. If you are a nurse, try to work in a facility that handles its staff well. Commit to a schedule that allows you to avoid overtime and lead a balanced and healthy life, leaving time and energy for your loved ones and your favorite entertainment.
- Support Groups- A system of support groups and colleagues provides a way to relieve frustration and discuss conflicts and challenges, so you can relax when you go home or on vacation. It can also improve teamwork and collaboration when you and your colleagues feel they are listening. If you are a tired nurse, desperate, depressed, or suffering from the symptoms of burnout, be sure to seek the help of a therapist or counselor.
- Changing Specialist- If your current area of expertise is too stressful, consider changing it. If you have your Nursing Degree, for example, a Master's Degree in Nursing or a PhD in Nursing will allow you to move to a specialty that suits you. Becoming a family nurse may increase the autonomy of your practice. Alternatively, you can consider teaching the next generation of clinicians as a nursing educator.
- Taking Breaks- Taking a short break from the tedious work helps in maintaining the burnout face out. To encourage this, institutions can introduce a mandatory vacation day policy with a quarterly check to ensure their staff are taking the time they need. This helps to increase job satisfaction and decrease the turnover rate among healthcare professionals.
What atre the Steps Concerning COVID-19?
Regarding individual measures, self-care is suggested as a line of defense for healthcare workers to manage requests for assistance of COVID-19 patients, especially when recovery times are short and long-term efforts are required. Physical activity, relaxation, balanced diet, good sleep hygiene, family support, meaningful relationships (also maintained through digital channels), job satisfaction, self-awareness through reflective practices, and small group discussions are the reported interventions with evidence of efficacy.
The counselors invite to support communication, even during busy periods, by (a) adopting a blame-free environment to share incidents, ethical or emergency issues, and challenges and advice; (b) involving nurses in management decisions (to promote a sense of togetherness and positivity where every voice has the opportunity to be heard); (c) allowing someone to talk before, during and after a shift. In addition, they recommend structuring a multidisciplinary team with psychologists, spiritual counselors, social professionals, and occupational health and safety physicians for professional psychosocial support to healthcare workers based on natural coping strategies (acceptance, active coping, positive framing). They also suggest creating a safe area to allow healthcare workers to quickly withdraw from an emotionally stressful situation and get peer support. The authors set time limits for shift periods (day and night and distinguish between light and intensive tasks) and frontline periods, alternating shift columns with holidays and vacationing when they occur. Finally, they report the importance of compensating health care workers through practical support such as social welfare for the care of children, the elderly, or animals.
Conclusion:
Brett H. Lewis said, 'Doctors diagnose, nurses heal, and caregivers make sense of it all'. Doctors are a huge part of our lives. They try to bring life and balance in our bodies but even they need to balance out their lives to ease their exhaustion and settle down a bit. They must follow various measures to maintain the burnout they face in their lives. Promising burnout treatment strategies included multidisciplinary activities involving alterations to the workplace environment and stress management courses that teach employees how to handle stressful situations better. However, there haven't been any thorough studies that demonstrate this as of yet. More interventional research focusing on medical students, residents, and practising physicians is required to enhance psychological well-being, career happiness, and patient care quality. Many studies highlighted the increase in the importance of work, enabling employees to participate in work-related decisions, show confidence in their abilities, work at a high level, promote goal achievement, and provide autonomy. This emphasizes the importance of leadership in creating a positive work environment. Also, improving the working conditions of nurses will attract more female nurses to the profession and allow them to stay in the profession longer.









