The Origin and the Backstory:
Clustered Regularly Interspaced Short Palindromic Repeats, or "CRISPR" (pronounced "crisper"), are a bacterial defense mechanism that serves as the foundation for the CRISPR-Cas9 genome editing technique. The term "CRISPR" or "CRISPR-Cas9" is frequently used informally in the field of genome engineering to refer to the numerous CRISPR-Cas9 and -CPF1 (and other) systems that can be programmed to target particular genetic code stretches and to edit DNA at precise locations, as well as for other uses, like developing new diagnostic tools. These technologies allow for the permanent modification of genes in living cells and animals. In the future, it may allow for correcting specific mutations in the human genome to treat diseases with genetic causes.
Researchers never imagined being able to change the genetic code of living cells so quickly and easily. CRISPR, which works like a pair of scissors to precisely delete, insert, or edit specific bits of DNA inside cells, makes this possible. This revolutionary gene-editing tool was discovered as a side project fueled by curiosity about how bacteria fight viruses. Drs. Jennifer Doudna and Emmanuelle Charpentier were awarded the Nobel Prize in Medicine in 2020 for their work on CRISPR. A year ago, the first US clinical trial of CRISPR-made cancer immunotherapy began, and more research is being conducted into CRISPR-made cancer treatments. Furthermore, trials are starting to test CRISPR directly in the body. While CRISPR is a game changer, it has limitations, and debate over the ethics of gene editing continues. But one thing is certain: CRISPR is a potent tool that has the potential to advance cancer research significantly and beyond.
In the last ten years, CRISPR has evolved from an acronym to a verb that has completely changed how biomedical research is conducted and how all elements of cell biology are studied. In the study of cancer, CRISPR and related methods have opened a window into issues that were once insurmountable in our knowledge of the noncoding genome, tumor heterogeneity, and the biology of cancer. They have also revealed fresh information on therapeutic vulnerabilities. CRISPR/Cas9 can be utilized in cancer research to modify genomes to investigate the mechanisms of carcinogenesis and development because genomic alterations in tumor cells cause cancer. With impressive outcomes, the CRISPR/Cas9 system has been utilized more frequently in recent years in cancer research and treatment.
Data Bridge Market Research analyses a growth rate in the global clustered regularly interspersed short palindromic repeats (CRISPR) market in the forecast period 2022-2029. The expected CAGR of global bone marrow biopsy market tends to be around 10.7% in the mentioned forecast period. The market was valued at USD 762.39 million in 2021, and it would grow upto USD 1719.33 million by 2029. North America is the dominating region due to the influential opportunities of an increasing inclination in biotechnology and pharmaceutical enterprises.
To know more about the study, visit: https://www.databridgemarketresearch.com/reports/global-clustered-regularly-interspersed-short-palindromic-repeats-crispr-market
CRISPR: A Technology that Occurred in 2013
The convenience offered by CRISPR has made it a mainstream technology in cancer and clinical, biological studies. Scientists have been looking for a simple technique to reverse these alterations by modifying DNA since they learned that mutations in DNA are the root cause of cancer. Although many gene editing techniques have been created over the years, none have matched the criteria for a quick, simple, and affordable technology. But in 2013, several studies revealed that a gene-editing tool known as CRISPR could modify the DNA of human cells like a finely tuned and simple pair of scissors. The new technology has dramatically changed what is possible and what is impossible in the scientific community. Cancer researchers leaped at the possibility of employing CRISPR as soon as it appeared on the shelves and freezers of labs worldwide.
CRISPR was inspired by nature, just like many other discoveries in science and health. In this instance, the concept was taken from a straightforward defense mechanism in some creatures, such as bacteria. These microorganisms seize bits of the intruder's DNA and store them away as segments known as CRISPRs, or clustered regularly interspersed short palindromic repeats, to defend themselves against invaders like viruses. These DNA fragments (converted into brief RNA fragments) aid an enzyme called Cas in locating and slicing up the invader's DNA if the same germ attempts to assault again.
When this defense mechanism was uncovered, researchers realized it could be used as a flexible gene-editing tool. Multiple groups successfully adapted the method to alter nearly any region of DNA within a few years, initially in the cells of other bacteria and eventually in human cells. Two key components make up the CRISPR tool in the lab: a guide RNA and a DNA-cutting enzyme, most frequently Cas9. Scientists create the guide RNA to mirror the DNA of the gene to be altered (called the target). In keeping with its name, the guide RNA teams up with Cas and directs Cas to the target. The DNA of the target gene is cut by Cas when the guide RNA and DNA align.
Depending on the CRISPR tool being used, the next step varies. In rare instances, the DNA of the target gene is damaged during repair, rendering the gene inactive. Other CRISPR variants allow for more precise gene editing, such as adding a new DNA segment or modifying a single DNA letter. Additionally, researchers have utilized CRISPR to find particular targets like RNA from cancer cells and DNA from viruses that cause cancer. CRISPR has most recently been used as an experimental test to find the new coronavirus. But the question is, how does CRISPR compare to other genome editing tools?
Other genome editing methods now in use are being replaced by CRISPR-Cas9, which is proving to be more effective and adaptable. As opposed to other tools, the CRISPR-Cas9 system does not require pairing with separate cleaving enzymes because it is capable of cutting DNA strands on its own. Additionally, they may be quickly paired with custom "guide" RNA (gRNA) sequences that will direct them to their DNA targets. These gRNA sequences have previously been produced in their tens of thousands and are available to the scientific community. Another feature that distinguishes CRISPR-Cas9 from other gene-editing techniques is its ability to target numerous genes simultaneously.
At the University of Pennsylvania, the first trial testing a CRISPR-created cancer medicine in the United States began in 2019. The research, which the NCI partially supports, examines a sort of immunotherapy in which the patient's own immune cells are genetically altered to more effectively "see" and eradicate their cancer. Four genetic alterations are made to T cells, immune cells with the ability to eradicate cancer, as part of the therapy.
First, the inclusion of a synthetic gene equips the T cells with a claw-like protein (referred to as a receptor) that can "see" the chemical NY-ESO-1 on some cancer cells. Then, three genes are deleted using CRISPR, two of which may interfere with the NY-ESO-1 receptor and one of which impairs the capacity of the cells to fight cancer. Large quantities of the end product, also known as NYCE T cells, were produced before being put into patients. This study set out to determine the safety of CRISPR-made therapy. Two patients with advanced multiple myeloma and one with metastatic sarcoma underwent testing. The T-cell therapy's target, NY-ESO-1, was present in the tumors of all three patients.
Initial research points to the treatment's safety. There were some side effects, but the researchers concluded that they were probably brought on by the chemotherapy the patients had previously had. There was no proof that the CRISPR-edited cells triggered an immunological response.
All four of the targeted genetic modifications were present in just about 10% of the T cells employed in the therapy. Additionally, all three patients' edited cells contained off-target alterations. Dr. Stadtmauer observed that none of the off-target edited cells expanded in a manner that suggested they had developed into cancer. The cancers in the patients barely changed as a result of the treatment. Two patients' tumors-one with multiple myeloma and the other with sarcoma-stopped growing for a period before starting again. For the third patient, the procedure had no effect at all.
Limitations of CRISPR
CRISPR has emerged as the preferred method for cancer researchers because of its advantages over other gene-editing techniques. There is also optimism that it will be useful in the treatment of cancer. But CRISPR has flaws, and because of these drawbacks, many scientists are hesitant to use it on humans.
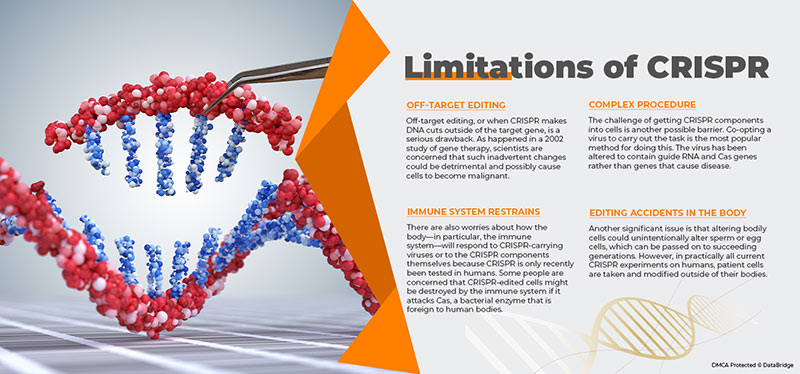
Fig: Limitations of CRISPR
- Off-Target Editing- Off-target editing, or when CRISPR makes DNA cuts outside of the target gene, is a serious drawback. As happened in a 2002 study of gene therapy, scientists are concerned that such inadvertent changes could be detrimental and possibly cause cells to become malignant. There is some worry that [CRISPR] could lead to cancer if it begins to damage random regions of the genome and cause the cell to begin putting things together in bizarre ways. However, researchers have increased CRISPR's capacity to selectively cut the intended target by modifying the Cas and guide RNA architectures.
- Complex Procedure- The challenge of getting CRISPR components into cells is another possible barrier. Co-opting a virus to carry out the task is the most popular method for doing this. The virus has been altered to contain guide RNA and Cas genes rather than genes that cause disease. It is one thing to introduce CRISPR into lab-grown cells, but quite another to do so in human bodily cells. Some CRISPR-carrying viruses can infect several cell types, so they might, for example, modify muscle cells while the intended target is liver cells. Researchers are looking into various strategies to precisely administer CRISPR to particular cells or organs in the human body. Viruses that solely affect one organ, such as the liver or brain, are being tested by some. Others have produced minuscule objects known as nano-capsules that are intended to deliver CRISPR elements to particular cells.
- Immune System Restrains- There are also worries about how the body—particularly the immune system—will respond to CRISPR-carrying viruses or to the CRISPR components themselves because CRISPR is only recently tested in humans. Some people are concerned that the immune system might destroy CRISPR-edited cells if it attacks Cas, a bacterial enzyme that is foreign to human bodies. A patient passed away twenty years ago as a result of his immune system's enormous onslaught on the viruses carrying the gene therapy he had gotten. Newer CRISPR-based strategies, on the other hand, rely on viruses that seem to be safer than those utilized in earlier gene treatments.
- Editing Accidents in the Body- Another significant issue is that altering bodily cells could unintentionally alter sperm or egg cells, which can be passed on to succeeding generations. However, in practically all current CRISPR experiments on humans, patient cells are taken and modified outside their bodies. Since it can be more precisely regulated than attempting to modify cells inside the body, the "ex vivo" method is thought to be safer. However, one ongoing study is exploring CRISPR gene editing directly in the eyes of individuals with Leber congenital amaurosis, a hereditary disorder that causes blindness.
The Conclusion and the Future:
CRISPR, pronounced "crisper," is a cutting-edge cancer treatment and gene-editing tool that fixes damaged DNA by cutting and sticking. Cuts in the DNA can turn off particular genes, eliminate cancer-causing mutations, or solve a production issue. Drug maker AbbVie and Caribou Biosciences declared in February 2021 that they would employ CRISPR to enhance CAR T-cell therapy, which genetically modifies a patient's T-cells (white blood cells) to combat cancer. It takes months, not a year or two, for CRISPR gene editing to genetically alter T cells, making it a potential new technology for cancer treatment. Patients may receive treatment considerably more quickly as a result.
Genetic medicine has ground-breaking potential. Modifying specific DNA sequences can change how your body fights cancer. This technology can give patients hope by increasing the specificity of the treatment and lowering the chance of cancer recurrence. Scientists can remove drug-resistance genes from tumor DNA. As a result, chemotherapy would be more effective and could prevent mutations from turning into aggressive malignancies, improving cancer patients' quality of life. Doctors might also use CRISPR technology to cut out the cancer-causing gene and screen patients for high-risk DNA abnormalities. 2019 saw the start of the initial CRISPR-based cancer clinical studies. They concentrated on enhancing current lung cancer therapies, including chemotherapy.
CRISPR enables researchers to modify DNA to enhance cancer treatment options or prevent cancer. In the future, more individualized treatment options and a better prognosis for cancer patients will be possible because to the expansion of genetic medicine. There are already ongoing clinical trials for more CRISPR-created cancer therapies. CRISPR-engineered CAR T-cell treatments are an additional type of immunotherapy that are being tested in a few trials. One business, for instance, is testing CRISPR-engineered CAR T cells on patients with multiple myeloma and B cell malignancies.
Regarding all the potential applications of CRISPR in cancer research and treatment, there are still a lot of unanswered questions. But one thing is certain: The industry is developing very quickly, and new uses for the technology are continually emerging.
The global CRISPR gene detection and diagnostic is supportive and aims to reduce the severity of the symptoms. Data Bridge Market Research analyses that the CRISPR gene detection and diagnostic market will grow at a CAGR of 19.5% from 2022 to 2029. The CRISPR gene detection and diagnostic market is segmented on the basis of six segments: class, products & services, application, workflow, end user, and distribution channel.
To know more about the study, visit: https://www.databridgemarketresearch.com/reports/global-crispr-gene-detection-and-diagnostic-market









