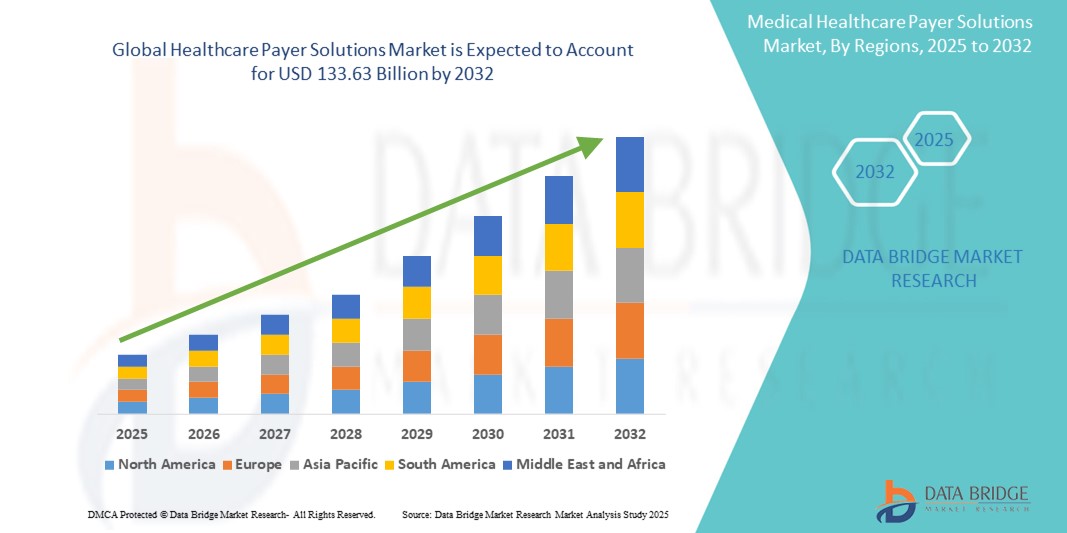
Global Healthcare Payer Solutions Market
市场规模(十亿美元)
CAGR :
% 
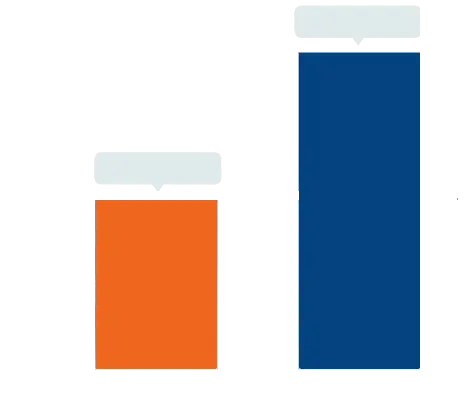 USD
72.19 Billion
USD
133.63 Billion
2024
2032
USD
72.19 Billion
USD
133.63 Billion
2024
2032
| 2025 –2032 | |
| USD 72.19 Billion | |
| USD 133.63 Billion | |
|
|
|
|
全球醫療保健付款人解決方案市場細分,按服務類型(業務流程外包、資訊技術外包和知識流程外包)、應用程式(索賠管理服務、綜合前台服務和後台運營、會員管理服務、提供者管理服務、計費和帳戶管理服務、分析和詐欺管理服務、人力資源服務、支付管理服務以及審計和分析系統)、最終用戶(私人付款
醫療保健付款人解決方案市場規模
- 2024 年全球醫療保健支付解決方案市場規模為721.9 億美元 ,預計 到 2032 年將達到 1,336.3 億美元,預測期內 複合年增長率為 8.00%。
- 市場擴張主要受醫療保健系統日益複雜的推動,以及對成本控制、索賠管理和增強患者參與度的需求日益增長,尤其是保險提供者和政府支付者
- 此外,進階分析、雲端平台和人工智慧工具的採用正在簡化營運並改善決策。這些創新正在改變傳統的支付模式,大大推動了對高效、可擴展的醫療保健支付解決方案的需求。
醫療保健支付者解決方案市場分析
- 醫療保健付款人解決方案涵蓋索賠管理、會員參與和風險評估的服務和平台,對於優化全球公共和私人保險組織的營運和提高成本效益至關重要
- 支付方解決方案需求的激增很大程度上是由於降低管理成本、改善患者治療效果以及遵守不斷發展的監管框架和基於價值的護理模式的壓力越來越大
- 北美在醫療保健支付解決方案市場佔據主導地位,2024 年的收入份額最高,為 46.8%,這得益於其高度數位化的醫療保健基礎設施、強有力的監管監督,以及保險公司和醫療保險和醫療補助等政府項目早期採用先進的分析和雲端技術
- 由於醫療保險覆蓋範圍的擴大、數位轉型措施以及印度和中國等國家的醫療保健支出不斷增加,預計亞太地區將成為預測期內醫療保健支付解決方案市場成長最快的地區
- 業務流程外包領域在醫療保健支付解決方案市場佔據主導地位,2024 年的市場份額為 50.1%,這得益於其成本效益、可擴展性以及簡化索賠處理和客戶支援等非核心管理職能的能力
報告範圍和醫療保健付款人解決方案市場細分
|
屬性 |
醫療保健付款人解決方案關鍵市場洞察 |
|
涵蓋的領域 |
|
|
覆蓋國家 |
北美洲
歐洲
亞太
中東和非洲
南美洲
|
|
主要市場參與者 |
|
|
市場機會 |
|
|
加值資料資訊集 |
除了對市場價值、成長率、細分、地理覆蓋範圍和主要參與者等市場情景的洞察之外,Data Bridge Market Research 策劃的市場報告還包括深入的專家分析、定價分析、品牌份額分析、消費者調查、人口統計分析、供應鏈分析、價值鏈分析、原材料/消耗品概述、供應商選擇標準、PESTLE 分析、波特分析和監管框架。 |
醫療保健支付解決方案市場趨勢
“索賠和會員管理中的人工智慧自動化和預測分析”
- 改變全球醫療保健支付解決方案市場的一大趨勢是將人工智慧(AI)、機器學習 (ML) 和預測分析融入支付系統,以簡化營運並提高決策準確性。這些技術越來越多地用於自動化理賠處理、偵測詐欺活動以及改善會員參與策略。
- 例如,Optum 和 Cognizant 等公司正在利用人工智慧實現重複性管理任務的自動化,從而減少處理時間和營運成本。人工智慧工具還可以分析大量資料集,預測醫療保健利用模式,使支付方能夠主動管理風險和護理結果。
- 預測分析可幫助付款人識別高風險成員,優化護理協調,並實現早期幹預,從而改善健康結果並降低成本。例如,Anthem, Inc. 使用資料分析對成員群體進行分層,並有效地指導資源分配。
- 聊天機器人和虛擬助理在會員服務功能中也變得越來越普遍,提供全天候支持,減少呼叫中心負載,並透過即時查詢解決提高用戶滿意度
- 這種向數位自動化和智慧化的轉變不僅提高了營運效率,而且使付款人系統與基於價值的護理、問責制和個人化會員體驗的更廣泛目標保持一致,從而推動了下一代付款人平台的持續創新和投資。
醫療保健支付解決方案市場動態
司機
“成本控制和法規遵循的需求不斷增長”
- 全球醫療保健支付者解決方案市場受到支付者日益增長的需求的推動,這些需求包括降低管理成本、確保及時處理索賠以及遵守不斷發展的醫療保健法規
- 例如,2024 年,CVS Health 宣布擴大其付款人解決方案組合,包括人工智慧驅動的索賠裁決和合規工具,旨在減輕行政負擔並提高索賠準確性
- 醫療支出的不斷增長和對基於價值的醫療服務的推動,促使公共和私人支付者採用數位平台來提高工作流程效率、減少詐欺並加強護理協調
- 此外,日益增長的政府授權和監管要求(例如 HIPAA、ICD-11 的採用和 ACA 合規性)進一步需要支援準確數據報告和即時審計的先進支付技術,從而推動已開發地區和新興地區的市場需求
克制/挑戰
“數據隱私問題和整合複雜性”
- 醫療保健支付解決方案市場面臨的主要挑戰之一是,在網路威脅日益增加以及 GDPR 和 HIPAA 等嚴格的資料保護法規日益嚴格的情況下,如何確保資料隱私和安全
- 健康數據系統中備受矚目的漏洞引起了利益相關者的警惕,需要建立強大的網路安全框架、安全的雲端基礎設施和全面的存取控制措施
- 此外,將付款方解決方案與傳統IT系統、分散的資料來源和提供者網路整合通常非常複雜且耗費資源。在許多情況下,組織在遷移到現代平台或整合分散的基礎設施時面臨技術和營運障礙。
- 這些整合困難,加上對系統停機、互通性和供應商鎖定的擔憂,可能會減緩傳統付款人的採用速度
- 透過可擴展、可互通的解決方案和明確的合規協議來克服這些挑戰對於市場的長期成功至關重要
醫療保健付款人解決方案市場範圍
市場根據服務類型、應用程式和最終用戶進行細分。
- 按服務類型
根據服務類型,醫療保健支付方解決方案市場細分為業務流程外包 (BPO)、資訊科技外包 (ITO) 和知識流程外包 (KPO)。業務流程外包 (BPO) 領域佔據市場主導地位,2024 年收入份額最高,達到 50.1%,這得益於透過外包理賠處理、會員服務和計費等服務來降低管理成本並提高營運效率的需求。支付方越來越多地採用 BPO 來簡化非核心流程、提高可擴展性並專注於核心策略功能。
預計知識流程外包 (KPO) 領域將在 2025 年至 2032 年期間實現最快成長,這得益於對高階分析、精算服務和風險管理解決方案日益增長的需求。隨著市場的成熟,支付方正在投資更高價值的外包服務,這些服務能夠提供數據驅動的洞察,並為策略決策提供支援。
- 按應用
根據應用,醫療保健支付方解決方案市場細分為理賠管理服務、整合前台服務和後台營運、會員管理服務、提供者管理服務、帳單和帳戶管理服務、分析和詐欺管理服務、人力資源服務、支付管理服務以及審計和分析系統。由於理賠量不斷增長以及對處理自動化、準確性和合規性的需求,理賠管理服務細分市場在2024年佔據了28.3%的最高市場份額。高效的理賠處理可顯著減少延誤和管理成本,使其成為私人和公共支付方關注的核心。
預計分析和詐欺管理服務領域將在2025年至2032年期間實現最快的複合年增長率,這得益於人們越來越重視透過預測分析和基於人工智慧的工具來檢測欺詐性索賠、管理風險以及改善成本控制。醫療保健數據日益複雜,也促使支付方在該領域採用智慧、可擴展的解決方案。
- 按最終用戶
根據最終用戶,醫療保健支付解決方案市場可細分為私人支付方和公共支付方。私人支付方佔據主導地位,2024 年的收入份額為 57.1%,這得益於其更高的投資能力、早期採用數位技術以及與第三方服務提供者日益增多的合作。私人保險公司在實施人工智慧、自動化和雲端解決方案方面更加靈活,進而提升效率和會員參與度。
在政府醫療改革、公共保險計劃的擴大以及利用整合數位平台對遺留系統進行現代化改造的舉措的支持下,公共付款人部門預計將在預測期內穩步增長。
醫療保健支付解決方案市場區域分析
- 北美在醫療保健支付解決方案市場佔據主導地位,2024 年的收入份額最高,為 46.8%,這得益於其高度數位化的醫療保健基礎設施、強有力的監管監督,以及保險公司和醫療保險和醫療補助等政府項目早期採用先進的分析和雲端技術
- 該地區專注於降低醫療成本、提高行政效率和遵守不斷變化的監管要求,正在加速採用數位支付解決方案,例如索賠自動化、詐欺檢測和會員參與工具
- 此外,熟練專業人員的可用性、優惠的政府政策和高額的醫療保健支出進一步支持私營和公共部門支付者解決方案的擴展,使北美成為該市場創新和實施的領先中心
美國醫療保健支付解決方案市場洞察
2024年,美國醫療保健支付解決方案市場佔據北美地區78.6%的最高收入份額,這得益於高昂的醫療支出、複雜的保險結構以及嚴格的監管。隨著醫療服務向價值導向轉變的日益加深、管理成本的不斷上升以及對改善會員診療結果的重視,對高級支付平台的需求也隨之增加。人工智慧、雲端系統和互通性工具的整合正在加速公共和私人支付方的數位轉型,從而促進市場擴張。
歐洲醫療保健支付解決方案市場洞察
受國家醫療改革、數位醫療解決方案日益普及以及控制公共醫療支出壓力的推動,歐洲醫療保健支付解決方案市場預計將在預測期內保持穩定的複合年增長率。德國、法國和英國等國家正在投資電子理賠管理、風險調整系統和人口健康分析,以實現支付方基礎設施的現代化。 《一般資料保護規範》(GDPR) 的實施也促進了該地區安全合規的支付方平台的開發。
英國醫療保健支付解決方案市場洞察
英國醫療保健支付方解決方案市場預計將穩定成長,這得益於英國國家醫療服務體系 (NHS) 的數位轉型措施以及降低營運效率的需求。政策驅動下,對整合醫療系統和基於價值的報銷模式的需求推動了支付方解決方案的採用。此外,對詐欺偵測和預測分析的日益關注也推動了政府和私人醫療機構的採用。
德國醫療保健支付解決方案市場洞察
德國醫療保健支付者解決方案市場正在不斷擴張,這得益於該國重視高效的法定醫療保險營運以及對嚴格監管框架的遵守。支付機構越來越多地採用自動化和人工智慧工具來簡化理賠流程、增強詐欺偵測能力並支援人口健康管理。德國強大的公私支付者組合和先進的醫療基礎設施使其成為歐洲整體市場成長的關鍵推動力。
亞太醫療保健支付解決方案市場洞察
預計亞太地區醫療保健支付解決方案市場將在2025年至2032年間以最快的複合年增長率增長,這得益於醫療支出的不斷增長、保險滲透率的不斷提升以及政府推動醫療數字化的舉措。中國、印度和日本等國家正在採用支付解決方案,以支持不斷擴大的國家保險計劃、提高理賠效率並減少詐欺。此外,對基於雲端和行動平台的日益關注也推動了區域市場的成長。
日本醫療保健支付解決方案市場洞察
日本的醫療保健支付解決方案市場正經歷強勁增長,這得益於該國全民醫療保健體系的現代化以及對高效理賠處理和分析的旺盛需求。由於日本人口老化導致成本上升,支付機構正在採用智慧解決方案來優化資源配置、偵測詐欺行為並確保服務的可持續交付。與電子病歷和數位健康平台的整合也正在蓬勃發展。
印度醫療保健支付解決方案市場洞察
2024年,印度佔據亞太地區最大的收入份額,這得益於其快速成長的健康保險業、數位健康使命計畫以及不斷擴大的公私合作夥伴關係。諸如「印度醫療援助計劃」(Ayushman Bharat)之類的政府項目正在推動對可擴展的雲端支付解決方案的需求,這些解決方案可用於管理理賠、會員數據和績效分析。醫療科技新創公司和價格實惠的IT服務的激增,進一步提升了印度作為支付解決方案充滿活力且潛力巨大的市場的地位。
醫療保健付款人解決方案市場份額
醫療保健支付解決方案產業主要由知名公司主導,包括:
- Optum, Inc.(美國)
- Cognizant(美國)
- 改變醫療保健(美國)
- ExlService Holdings, Inc.(美國)
- 印孚瑟斯有限公司(印度)
- 塔塔諮詢服務有限公司(印度)
- Wipro(印度)
- 埃森哲(愛爾蘭)
- IBM(美國)
- Conduent Incorporated(美國)
- HCL Technologies Limited(印度)
- NTT DATA集團公司(日本)
- Atos SE(法國)
- DXC科技公司(美國)
- Genpact有限公司(美國)
- 甲骨文公司(美國)
- Epic Systems Corporation(美國)
- HealthEdge Software, Inc.(美國)
- Inovalon Holdings, Inc.(美國)
- 麥克森公司(美國)
全球醫療保健支付解決方案市場的最新發展是什麼?
- 2024年4月,聯合健康集團旗下領先的醫療服務供應商Optum推出了新一代人工智慧理賠裁決引擎,旨在加快處理速度並減少錯誤。該解決方案整合了預測分析功能,可以標記異常情況,增強詐欺偵測能力並提高報銷準確性。這項進展體現了Optum致力於推進醫療保健支付方營運自動化和數據智慧化的決心。
- 2024年3月,Cognizant Technology Solutions 擴展了其醫療支付平台,新增了專注於法規遵循和基於價值的報銷模式的功能。此次升級包括增強的互通性功能,從而能夠更好地與電子健康記錄和健康資訊交換進行整合。此舉鞏固了 Cognizant 在為私人和公共支付者提供可擴展、合規解決方案方面的地位。
- 2024年2月,Change Healthcare(現隸屬於Optum)推出了一個先進的支付準確性平台,幫助付款人在理賠前識別並防止超額支付。該平台利用即時分析和人工智慧演算法,顯示付款人生態系統對智慧成本控制工具的需求日益增長。
- 2024年1月,印孚瑟斯公司宣布與一家領先的美國健康保險公司建立策略合作夥伴關係,利用雲端原生架構對其核心付款系統進行現代化升級。此次合作旨在透過全面整合的數位化解決方案,提升會員體驗、即時理賠追蹤和營運敏捷性。
- 2023年12月,EXL Service Holdings Inc. 推出了一款專用的醫療保健支付方分析套件,旨在支援人口健康管理和風險分層。該解決方案使支付方能夠從海量醫療保健數據集中獲得切實可行的洞察,從而支持改進護理協調和基於結果的規劃,彰顯了行業向數據驅動戰略轉型的趨勢。
SKU-
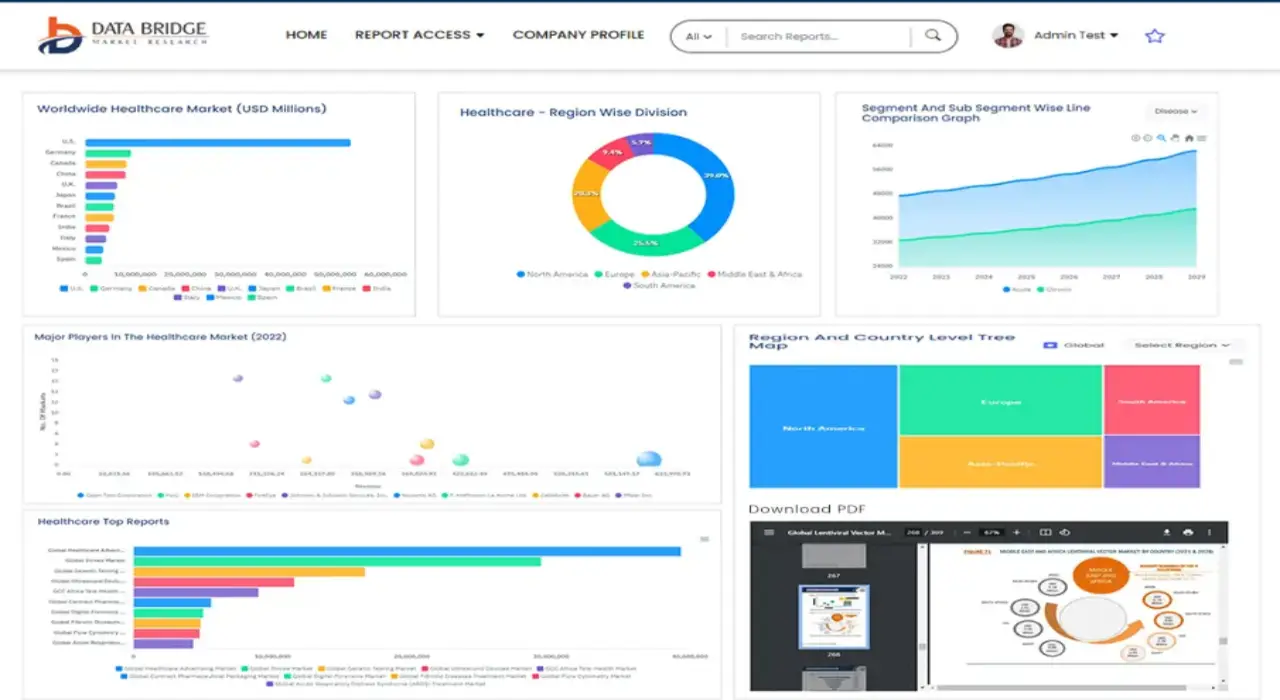
Get online access to the report on the World's First Market Intelligence Cloud
- Interactive Data Analysis Dashboard
- Company Analysis Dashboard for high growth potential opportunities
- Research Analyst Access for customization & queries
- Competitor Analysis with Interactive dashboard
- Latest News, Updates & Trend analysis
- Harness the Power of Benchmark Analysis for Comprehensive Competitor Tracking
目录
1 INTRODUCTION
1.1 OBJECTIVES OF THE STUDY
1.2 MARKET DEFINITION
1.3 OVERVIEW OF GLOBAL HEALTHCARE PAYER SOLUTIONS MARKET
1.4 CURRENCY AND PRICING
1.5 LIMITATION
1.6 MARKETS COVERED
2 MARKET SEGMENTATION
2.1 KEY TAKEAWAYS
2.2 ARRIVING AT THE GLOBAL HEALTHCARE PAYER SOLUTIONS MARKET SIZE
2.2.1 VENDOR POSITIONING GRID
2.2.2 TECHNOLOGY LIFE LINE CURVE
2.2.3 TRIPOD DATA VALIDATION MODEL
2.2.4 MARKET GUIDE
2.2.5 MULTIVARIATE MODELLING
2.2.6 TOP TO BOTTOM ANALYSIS
2.2.7 CHALLENGE MATRIX
2.2.8 APPLICATION COVERAGE GRID
2.2.9 STANDARDS OF MEASUREMENT
2.2.10 VENDOR SHARE ANALYSIS
2.2.11 DATA POINTS FROM KEY PRIMARY INTERVIEWS
2.2.12 DATA POINTS FROM KEY SECONDARY DATABASES
2.3 GLOBAL HEALTHCARE PAYER SOLUTIONS MARKET: RESEARCH SNAPSHOT
2.4 ASSUMPTIONS
3 MARKET OVERVIEW
3.1 DRIVERS
3.2 RESTRAINTS
3.3 OPPORTUNITIES
3.4 CHALLENGES
4 EXECUTIVE SUMMARY
5 PREMIUM INSIGHTS
5.1 PESTEL ANALYSIS
5.2 PORTER’S FIVE FORCES MODEL
6 INDUSTRY INSIGHTS
6.1 KEY PRICING STRATEGIES
6.2 DATA-DRIVEN DECISION MAKING
6.3 ADOPTION OF OUTSOURCING
6.4 INTERVIEWS WITH SPECIALIST
6.5 OTHER KOL SNAPSHOTS
6.6 PAYER VALUE CHAIN ANALYSIS
7 MERGERS AND ACQUISITION
7.1 LICENSING
7.2 COMMERCIALIZATION AGREEMENTS
8 REGULATORY FRAMEWORK
8.1 REGULATORY PROCESS
8.2 REGULATORY APPROVAL PATHWAYS
8.3 LICENSING AND REGISTRATION
9 MARKET ACCESS
9.1 10-YEAR MARKET FORECAST
9.2 TECHNOLOGICAL ENABLEMENT
9.3 EXPANDING HEALTH INSURANCE COVERAGE
9.4 FOCUS ON CUSTOMER ENGAGEMENT
9.5 NAVIGATING REIMBURSEMENT MODELS
10 MARKET OVERVIEW
10.1 DRIVERS
10.2 RESTRAINTS
10.3 OPPORTUNITIES
10.4 CHALLENGES
11 GLOBAL HEALTHCARE PAYER SOLUTIONS MARKET , BY SERVICE TYPE
11.1 OVERVIEW
11.2 BUSINESS PROCESS OUTSOURCING
11.2.1 CLAIMS PROCESSING
11.2.2 CUSTOMER SERVICE
11.2.3 ENROLLMENT & BILLING SERVICES
11.2.4 PROVIDER MANAGEMENT
11.2.5 MEDICAL CODING & BILLING
11.2.6 OTHER ADMINISTRATIVE SERVICES
11.3 KPO (KNOWLEDGE PROCESS OUTSOURCING)
11.3.1 DATA ANALYTICS & ACTUARIAL SERVICES
11.3.2 COMPLIANCE & RISK MANAGEMENT
11.3.3 FRAUD DETECTION & PREVENTION
11.3.4 HEALTHCARE CONSULTING & MARKET RESEARCH
11.3.5 HEALTH PLAN DESIGN & CONSULTING
11.3.6 PREDICTIVE MODELING
11.4 ITO (INFORMATION TECHNOLOGY OUTSOURCING)
11.4.1 IT INFRASTRUCTURE MANAGEMENT
11.4.2 APPLICATION MANAGEMENT SERVICES
11.4.3 CYBERSECURITY & DATA PRIVACY
11.4.4 CLOUD SERVICES & HOSTING
11.4.5 SYSTEM INTEGRATION & IMPLEMENTATION
11.4.6 DATA WAREHOUSING & BUSINESS INTELLIGENCE
12 GLOBAL HEALTHCARE PAYER SOLUTIONS MARKET , BY APPLICATION
12.1 OVERVIEW
12.2 CLAIMS MANAGEMENT
12.3 PROVIDER NETWORK MANAGEMENT
12.4 CUSTOMER RELATIONSHIP MANAGEMENT
12.5 BILLING & ACCOUNTS MANAGEMENT
12.6 COMPLIANCE MANAGEMENT
12.7 FRAUD DETECTION & PREVENTION
12.8 DATA ANALYTICS & HEALTH INFORMATICS
13 GLOBAL HEALTHCARE PAYER SOLUTIONS MARKET , BY DEPLOYMENT MODE
13.1 OVERVIEW
13.2 ON-PREMISE
13.3 CLOUD-BASED
14 GLOBAL HEALTHCARE PAYER SOLUTIONS MARKET , BY END USER
14.1 OVERVIEW
14.2 PRIVATE PAYERS
14.2.1 INSURANCE COMPANIES
14.2.2 HEALTH MAINTENANCE ORGANIZATIONS (HMOS)
14.2.3 PREFERRED PROVIDER ORGANIZATIONS (PPOS)
14.3 PUBLIC PAYERS
14.3.1 GOVERNMENT HEALTH INSURANCE PROGRAMS
14.3.2 MEDICARE & MEDICAID
15 GLOBAL HEALTHCARE PAYER SOLUTIONS MARKET , BY CONTRACT TYPE
15.1 OVERVIEW
15.2 LONG-TERM CONTRACTS
15.3 SHORT-TERM CONTRACTS
16 GLOBAL HEALTHCARE PAYER SOLUTIONS MARKET , BY SIZE OF ORGANIZATION (PAYER)
16.1 OVERVIEW
16.2 LARGE ENTERPRISES
16.3 SMALL & MEDIUM ENTERPRISES (SMES)
17 GLOBAL HEALTHCARE PAYER SOLUTIONS MARKET , SWOT AND DBMR ANALYSIS
18 GLOBAL HEALTHCARE PAYER SOLUTIONS MARKET , COMPANY LANDSCAPE
18.1 COMPANY SHARE ANALYSIS: GLOBAL
18.2 COMPANY SHARE ANALYSIS: NORTH AMERICA
18.3 COMPANY SHARE ANALYSIS: EUROPE
18.4 COMPANY SHARE ANALYSIS: ASIA-PACIFIC
18.5 MERGERS & ACQUISITIONS
18.6 NEW PRODUCT DEVELOPMENT & APPROVALS
18.7 EXPANSIONS
18.8 REGULATORY CHANGES
18.9 PARTNERSHIP AND OTHER STRATEGIC DEVELOPMENTS
19 GLOBAL HEALTHCARE PAYER SOLUTIONS MARKET , BY REGION
GLOBAL HEALTHCARE PAYER SOLUTIONS MARKET , (ALL SEGMENTATION PROVIDED ABOVE IS REPRESENTED IN THIS CHAPTER BY COUNTRY)
19.1 NORTH AMERICA
19.1.1 U.S.
19.1.2 CANADA
19.1.3 MEXICO
19.2 EUROPE
19.2.1 GERMANY
19.2.2 U.K.
19.2.3 ITALY
19.2.4 FRANCE
19.2.5 SPAIN
19.2.6 RUSSIA
19.2.7 SWITZERLAND
19.2.8 TURKEY
19.2.9 BELGIUM
19.2.10 NETHERLANDS
19.2.11 DENMARK
19.2.12 SWEDEN
19.2.13 POLAND
19.2.14 NORWAY
19.2.15 FINLAND
19.2.16 REST OF EUROPE
19.3 ASIA-PACIFIC
19.3.1 JAPAN
19.3.2 CHINA
19.3.3 SOUTH KOREA
19.3.4 INDIA
19.3.5 SINGAPORE
19.3.6 THAILAND
19.3.7 INDONESIA
19.3.8 MALAYSIA
19.3.9 PHILIPPINES
19.3.10 AUSTRALIA
19.3.11 NEW ZEALAND
19.3.12 VIETNAM
19.3.13 TAIWAN
19.3.14 REST OF ASIA-PACIFIC
19.4 SOUTH AMERICA
19.4.1 BRAZIL
19.4.2 ARGENTINA
19.4.3 REST OF SOUTH AMERICA
19.5 MIDDLE EAST AND AFRICA
19.5.1 SOUTH AFRICA
19.5.2 EGYPT
19.5.3 BAHRAIN
19.5.4 UNITED ARAB EMIRATES
19.5.5 KUWAIT
19.5.6 OMAN
19.5.7 QATAR
19.5.8 SAUDI ARABIA
19.5.9 REST OF MEA
19.6 KEY PRIMARY INSIGHTS: BY MAJOR COUNTRIES
20 GLOBAL HEALTHCARE PAYER SOLUTIONS MARKET , COMPANY PROFILE
20.1 COGNIZANT
20.1.1 COMPANY OVERVIEW
20.1.2 REVENUE ANALYSIS
20.1.3 GEOGRAPHIC PRESENCE
20.1.4 PRODUCT PORTFOLIO
20.1.5 RECENT DEVELOPMENTS
20.2 ACCENTURE
20.2.1 COMPANY OVERVIEW
20.2.2 REVENUE ANALYSIS
20.2.3 GEOGRAPHIC PRESENCE
20.2.4 PRODUCT PORTFOLIO
20.2.5 RECENT DEVELOPMENTS
20.3 XEROX (CONDUENT)
20.3.1 COMPANY OVERVIEW
20.3.2 REVENUE ANALYSIS
20.3.3 GEOGRAPHIC PRESENCE
20.3.4 PRODUCT PORTFOLIO
20.3.5 RECENT DEVELOPMENTS
20.4 TATA CONSULTANCY SERVICES (TCS)
20.4.1 COMPANY OVERVIEW
20.4.2 REVENUE ANALYSIS
20.4.3 GEOGRAPHIC PRESENCE
20.4.4 PRODUCT PORTFOLIO
20.4.5 RECENT DEVELOPMENTS
20.5 WIPRO
20.5.1 COMPANY OVERVIEW
20.5.2 REVENUE ANALYSIS
20.5.3 GEOGRAPHIC PRESENCE
20.5.4 PRODUCT PORTFOLIO
20.5.5 RECENT DEVELOPMENTS
20.6 INFOSYS
20.6.1 COMPANY OVERVIEW
20.6.2 REVENUE ANALYSIS
20.6.3 GEOGRAPHIC PRESENCE
20.6.4 PRODUCT PORTFOLIO
20.6.5 RECENT DEVELOPMENTS
20.7 UNITEDHEALTH GROUP (OPTUM)
20.7.1 COMPANY OVERVIEW
20.7.2 REVENUE ANALYSIS
20.7.3 GEOGRAPHIC PRESENCE
20.7.4 PRODUCT PORTFOLIO
20.7.5 RECENT DEVELOPMENTS
20.8 HCL TECHNOLOGIES
20.8.1 COMPANY OVERVIEW
20.8.2 REVENUE ANALYSIS
20.8.3 GEOGRAPHIC PRESENCE
20.8.4 PRODUCT PORTFOLIO
20.8.5 RECENT DEVELOPMENTS
20.9 EXL SERVICE HOLDINGS, INC.
20.9.1 COMPANY OVERVIEW
20.9.2 REVENUE ANALYSIS
20.9.3 GEOGRAPHIC PRESENCE
20.9.4 PRODUCT PORTFOLIO
20.9.5 RECENT DEVELOPMENTS
20.1 IBM CORPORATION
20.10.1 COMPANY OVERVIEW
20.10.2 REVENUE ANALYSIS
20.10.3 GEOGRAPHIC PRESENCE
20.10.4 PRODUCT PORTFOLIO
20.10.5 RECENT DEVELOPMENTS
20.11 GENPACT
20.11.1 COMPANY OVERVIEW
20.11.2 REVENUE ANALYSIS
20.11.3 GEOGRAPHIC PRESENCE
20.11.4 PRODUCT PORTFOLIO
20.11.5 RECENT DEVELOPMENTS
20.12 NTT DATA CORPORATION
20.12.1 COMPANY OVERVIEW
20.12.2 REVENUE ANALYSIS
20.12.3 GEOGRAPHIC PRESENCE
20.12.4 PRODUCT PORTFOLIO
20.12.5 RECENT DEVELOPMENTS
20.13 MPHASIS
20.13.1 COMPANY OVERVIEW
20.13.2 REVENUE ANALYSIS
20.13.3 GEOGRAPHIC PRESENCE
20.13.4 PRODUCT PORTFOLIO
20.13.5 RECENT DEVELOPMENTS
20.14 CAPGEMINI
20.14.1 COMPANY OVERVIEW
20.14.2 REVENUE ANALYSIS
20.14.3 GEOGRAPHIC PRESENCE
20.14.4 PRODUCT PORTFOLIO
20.14.5 RECENT DEVELOPMENTS
20.15 WNS GLOBAL SERVICES
20.15.1 COMPANY OVERVIEW
20.15.2 REVENUE ANALYSIS
20.15.3 GEOGRAPHIC PRESENCE
20.15.4 PRODUCT PORTFOLIO
20.15.5 RECENT DEVELOPMENTS
20.16 HGS (HINDUJA GLOBAL SOLUTIONS)
20.16.1 COMPANY OVERVIEW
20.16.2 REVENUE ANALYSIS
20.16.3 GEOGRAPHIC PRESENCE
20.16.4 PRODUCT PORTFOLIO
20.16.5 RECENT DEVELOPMENTS
20.17 SUTHERLAND GLOBAL SERVICES
20.17.1 COMPANY OVERVIEW
20.17.2 REVENUE ANALYSIS
20.17.3 GEOGRAPHIC PRESENCE
20.17.4 PRODUCT PORTFOLIO
20.17.5 RECENT DEVELOPMENTS
20.18 SUTHERLAND GLOBAL SERVICES
20.18.1 COMPANY OVERVIEW
20.18.2 REVENUE ANALYSIS
20.18.3 GEOGRAPHIC PRESENCE
20.18.4 PRODUCT PORTFOLIO
20.18.5 RECENT DEVELOPMENTS
20.19 HEXAWARE TECHNOLOGIES
20.19.1 COMPANY OVERVIEW
20.19.2 REVENUE ANALYSIS
20.19.3 GEOGRAPHIC PRESENCE
20.19.4 PRODUCT PORTFOLIO
20.19.5 RECENT DEVELOPMENTS
20.2 CONCENTRIX
20.20.1 COMPANY OVERVIEW
20.20.2 REVENUE ANALYSIS
20.20.3 GEOGRAPHIC PRESENCE
20.20.4 PRODUCT PORTFOLIO
20.20.5 RECENT DEVELOPMENTS
20.21 ALORICA
20.21.1 COMPANY OVERVIEW
20.21.2 REVENUE ANALYSIS
20.21.3 GEOGRAPHIC PRESENCE
20.21.4 PRODUCT PORTFOLIO
20.21.5 RECENT DEVELOPMENTS
20.22 FIRSTSOURCE SOLUTIONS
20.22.1 COMPANY OVERVIEW
20.22.2 REVENUE ANALYSIS
20.22.3 GEOGRAPHIC PRESENCE
20.22.4 PRODUCT PORTFOLIO
20.22.5 RECENT DEVELOPMENTS
20.23 DXC TECHNOLOGY
20.23.1 COMPANY OVERVIEW
20.23.2 REVENUE ANALYSIS
20.23.3 GEOGRAPHIC PRESENCE
20.23.4 PRODUCT PORTFOLIO
20.23.5 RECENT DEVELOPMENTS
21 RELATED REPORTS
22 CONCLUSION
23 QUESTIONNAIRE
24 ABOUT DATA BRIDGE MARKET RESEARCH

研究方法
数据收集和基准年分析是使用具有大样本量的数据收集模块完成的。该阶段包括通过各种来源和策略获取市场信息或相关数据。它包括提前检查和规划从过去获得的所有数据。它同样包括检查不同信息源中出现的信息不一致。使用市场统计和连贯模型分析和估计市场数据。此外,市场份额分析和关键趋势分析是市场报告中的主要成功因素。要了解更多信息,请请求分析师致电或下拉您的询问。
DBMR 研究团队使用的关键研究方法是数据三角测量,其中包括数据挖掘、数据变量对市场影响的分析和主要(行业专家)验证。数据模型包括供应商定位网格、市场时间线分析、市场概览和指南、公司定位网格、专利分析、定价分析、公司市场份额分析、测量标准、全球与区域和供应商份额分析。要了解有关研究方法的更多信息,请向我们的行业专家咨询。
可定制
Data Bridge Market Research 是高级形成性研究领域的领导者。我们为向现有和新客户提供符合其目标的数据和分析而感到自豪。报告可定制,包括目标品牌的价格趋势分析、了解其他国家的市场(索取国家列表)、临床试验结果数据、文献综述、翻新市场和产品基础分析。目标竞争对手的市场分析可以从基于技术的分析到市场组合策略进行分析。我们可以按照您所需的格式和数据样式添加您需要的任意数量的竞争对手数据。我们的分析师团队还可以为您提供原始 Excel 文件数据透视表(事实手册)中的数据,或者可以帮助您根据报告中的数据集创建演示文稿。