The most prevalent medical problem in women of reproductive age is obesity. Pregnant women's obesity statistics are rising in the United States. According to the Centers for Disease Control and Prevention, 29% of pregnant women in 2019 had obesity at the start of their pregnancies, a 3% rise from 2016. Obesity can have a negative impact on all aspects of the reproductive cycle, including the inability to conceive, difficulties during labor and delivery, and breastfeeding challenges. Babies born to obese moms are also more likely to become overweight or obese as adults. Obese women may require antenatal treatment with known hypertension; some may also have type 2 diabetes without a diagnosis. Other issues crop up later in the pregnancy, during birth, or after delivery. Obesity is linked to an increased risk of suboptimal pregnancy outcomes and of maternal and infant death, but most obese pregnant women are quite unaware of the problems they face.
Obesity is linked to an increased risk of almost all pregnancy complications. Women with an obese BMI are more likely to experience congenital defects, gestational diabetes mellitus (GDM), gestational hypertension, preeclampsia, delivery of a large-for-gestational-age baby, and other complications during pregnancy. Additionally, many more cesarean sections are performed, and anesthesia may not be ideal. The less common cases of gastroschisis and spontaneous preterm labor are notable outliers. Obese women frequently struggle to start and maintain breastfeeding.
Our DBMR team investigated the preeclampsia drugs market and witnessed that the expected CAGR of preeclampsia drugs market is tend to be around 10% in the mentioned forecast period. America dominates the market in the forecast period due to the growing recognition among patients and health care providers about the seriousness of the disease. Asia-Pacific is considered the most lucrative period due to increased healthcare spending and the adoption of technologically advanced medicines which will increase the preeclampsia drugs market growth in the region.
To know more about the study, kindly visit: https://www.databridgemarketresearch.com/reports/global-preeclampsia-drugs-market
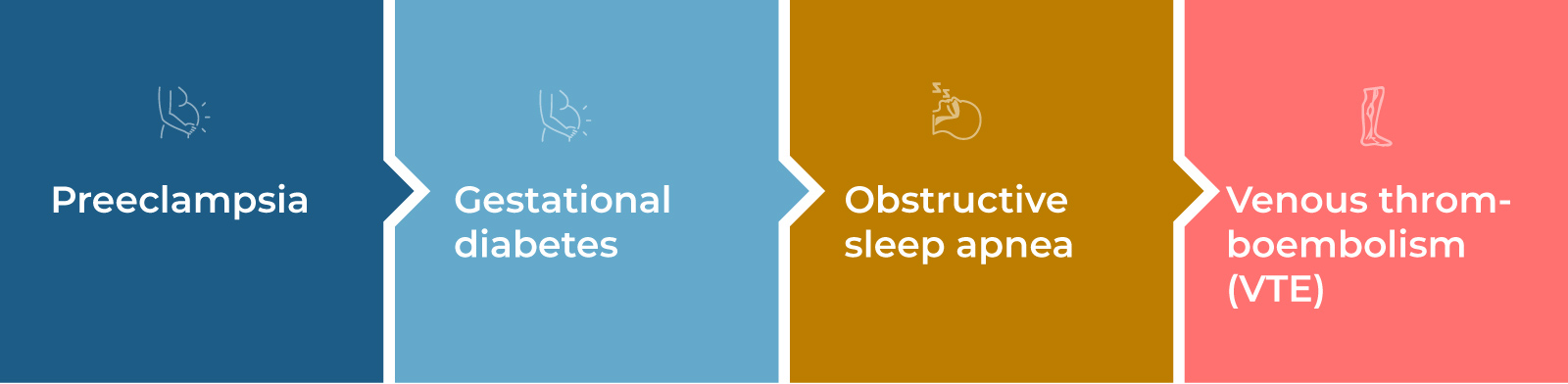
Risks of Obesity During Pregnancy for the Mother
Obesity during pregnancy can lead to the huge risk of developing approximately all pregnancy complications. These can lead to early delivery or long-term health problems.
- Preeclampsia is a serious form of gestational hypertension (high blood pressure) that generally happens in the second half of pregnancy or soon after childbirth. The condition can cause organ failure and, in some extreme rare cases, seizures, heart attack, or stroke.
- Gestational diabetes- Increased glucose or blood sugar levels increase the chance of a cesarean birth and having a very large baby. Women who have had gestational diabetes have a higher risk of developing diabetes in the future, as do their children.
- Obstructive sleep apnea- During pregnancy, sleep apnea, in which breathing repeatedly stops and starts, can cause fatigue and increase the risk of high blood pressure and heart and lung problems.
- Venous thromboembolism (VTE) occurs when a blood clot breaks off in the leg or arm and travels to vital organs, potentially causing a stroke or heart attack.
Our DBMR team investigated the global venous thromboembolism market and witnessed that the expected CAGR of global venous thromboembolism market is tend to be around 8.50% in the mentioned forecast period. Asia-Pacific dominates the market due to the increased prevalence of embolism and the increasing geriatric population. Further, the geriatric population is expected to increase the patient population globally, which boots the global venous thromboembolism market in the forecast period.
To know more about the study, kindly visit: https://www.databridgemarketresearch.com/reports/global-venous-thromboembolism-market
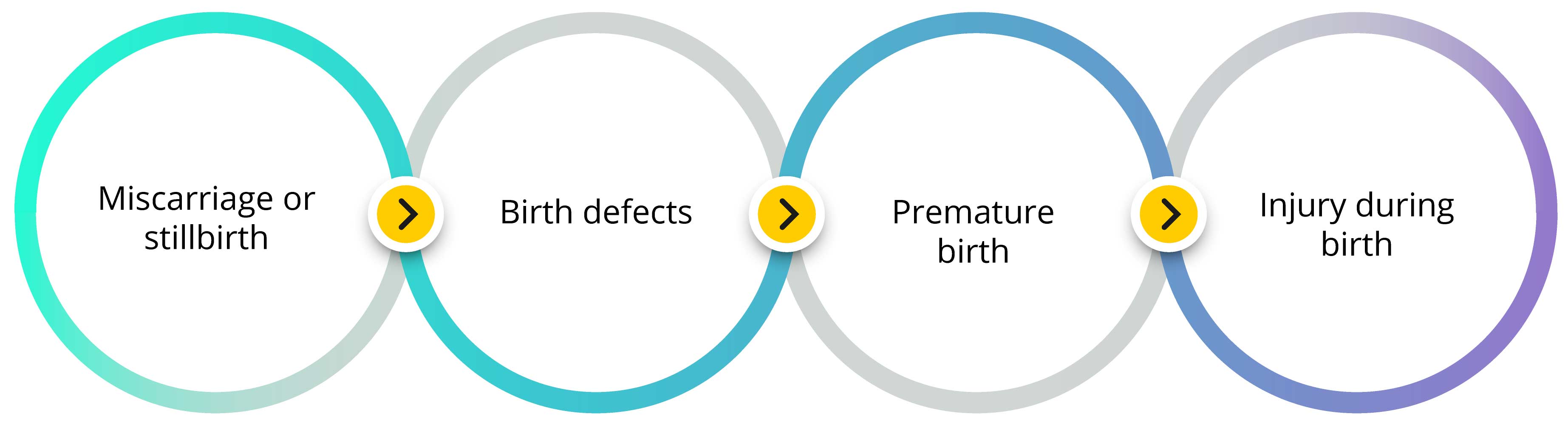
Risks of Obesity During Pregnancy for the Baby
Obesity during pregnancy poses a number of risks to the gestating child. Babies carried by a mother with obesity have a greater chance of:
- Miscarriage or Stillbirth
- Birth Defects Include Heart and neural tube defects, such as spina bifida. Moreover, it can be more difficult for healthcare providers to identify such defects in utero due to excess body fat obstructing an ultrasound exam.
- Premature Birth- It develops as a result of maternal conditions, such as preeclampsia. Preterm babies are at higher risk of problems with eating, breathing, and staying warm.
- Injury During Birth- It happens because the baby is much larger than average (macrosomia which is generally defined as birth weight greater than 8 pounds, 13 ounces)
Now, for everything there is an ideal parameter. Likewise, here too, there is an ideal weight that doctors recommend which is most suitable for the mother during pregnancy.
According to Centers for Disease Control and Prevention (CDC), these are the recommended amounts of weight one should gain:
- If BMI is less than 18.5, one should aim to gain 28-40 pounds
- If BMI is 18.5-24.9, one should aim to gain 25-35 pounds
- If BMI is 25-29.9, one should aim to gain 15-25 pounds
- If BMI is 30 or higher, one should aim to gain 11-20 pounds
Care for Pregnant Obese Patients
- Antepartum Care
The risk of hypertensive diseases of pregnancy, most notably preeclampsia, is increased in mothers with obesity. Some studies cite a 3–10 fold increase in preeclampsia risk compared to normal weight women. The higher preeclampsia risk appears to show a dose-response relationship, with one study finding that the risk for preeclampsia doubles with each 5 kg/m2 increase in BMI. Regardless of chronic hypertension, it is advised to all pregnant obese women to get baseline labs and urine protein creatinine ratios. In addition, due to their elevated risk of cardiomyopathy and underlying vascular illness, we advise women with class III and super-obesity to take into account a baseline transthoracic echo.
The United States Preventative Services Task Force (USPSTF) believes that the present evidence does not support screening for gestational diabetes (GDM) before 24 weeks of gestation in asymptomatic pregnant women. (26). The USPSTF acknowledges that a clinician should use their clinical judgement when deciding what screening is appropriate for a patient in the first or early second trimester who has type 2 diabetes risk factors (obesity, family history of diabetes, or foetal macrosomia in a prior pregnancy).
- Intrapartum
For women with obesity, a multi-disciplinary approach to their intrapartum care is required; for patients with a BMI >40 kg/m2, consultation with specialists should be considered; for those patients with a BMI >50 kg/m2, it is highly recommended. Further, a multi-disciplinary care team should include Maternal-Fetal Medicine (MFM) specialists in nursing and, pharmacy, Anesthesia, with proper consultation with Critical Care, Cardiology, and Pulmonology colleagues.
- Physical room, accommodating equipment created for patients with obesity, and personnel with experience transferring bariatric patients are all crucial for the bariatric patient. Obtaining a bariatric bed and surgical table is essential. If the patient is to undergo surgery, putting a hover on the bed in advance will help with any upcoming transfers. Bariatric wheelchairs and commodes, large surgical safety straps, and sequential compression devices are additional factors to consider.
- Prior to admission, obstetric anesthesia specialists should meet with the patient to review comorbidities, gauge pulmonary and cardiovascular health, and perform an airway exam. This is also a chance to ask about previous difficult neuraxial placements or airway situations. During the consultation, a discussion of labor analgesic options, such as labor epidurals, and anesthetic options for cesarean deliveries should also be covered. The placement of labor epidurals can be more challenging, take longer to place, and are more likely to need replacement in obese patients, so early labor epidural placement should be taken into consideration. When the patient chooses a vaginal delivery, having an early epidural placed, adequate access to anesthesiologists, extra staff to help with transfers, and fiber optic equipment for possible urgent intubation is recommended.
IV access is an important part of labor and delivery and must be approached to obtain access with minimal discomfort to the patient. Several attempts to start an IV should prompt the request for additional resources, which includes ultrasound guided placement, and consideration for peripherally inserted central catheters.
- Ultrasound assessment for fetal presentation may be important, and a vaginal exam may be inadequate to evaluate fetal presentation in the context of obesity. At times, fetal monitoring is not feasible when body habitus restricts the ability of cardiotocography to pick up fetal heart rate. Many a time, the tissue penetration of a curvilinear probe may be inadequate, and an endovaginal probe can be used transabdominal, often in the umbilicus, to obtain imaging because of decreased umbilical tissue thickness.
Our DBMR team investigated the fetal monitoring market and witnessed that the market was valued at USD 3.32 billion in 2021 and is expected to reach USD 5.45 billion by 2029, registering a CAGR of 6.40% during the forecast period of 2022 to 2029. Asia-Pacific dominates the fetal monitoring market because of the increasing expenditure of healthcare infrastructure and growing adoption of advanced dental technologies in this region.
To know more about the study, kindly visit: https://www.databridgemarketresearch.com/reports/global-fetal-monitoring-market
- A nurse must remain at bedside to adjust the external fetal monitor and palpate for contractions. Intermittent ultrasound of the fetal heart rate transabdominal could be performed, but is not an evidence-based recommendation, as a meta-analysis of studies evaluating intermittent auscultation vs. continuous monitoring often excluded high risk pregnancies
Surgical Care
Obesity, and particularly super obesity, has been associated with increased rates of post-cesarean complications. The increasing risk of post-cesarean wound complications mirrors an increasing BMI, with higher complication rates seen in women with higher BMIs, and there is a 30–50% risk of wound complications in women with super-obesity. It is highly recommended that all women undergoing cesarean delivery receive broad spectrum antibiotics. Since women with super obesity are at higher risk of postpartum endometritis, with rates projected at 3–8%, vaginal preparation should be considered, especially in those women with ruptured membranes.
Postpartum Care
An online application describes nursing care strategies for secure patient handling in the context of obesity and super-obesity. Safe transfers, positioning adjustments, access to the abdominal and perineal regions, bathing and showering, and floor/fall recovery are just a few of the topics covered in this resource. A bariatric bed and bariatric lift may be needed for the super obese patient during the postpartum period to increase staff safety while caring for them. In the population of people who are extremely obese, there is a 1-2% risk of maternal intensive care unit admission for women who give birth via cesarean section. Depending on the specific patient and delivery characteristics, an ICU setting may be required for initial post-operative recovery. Increased nursing-to-patient ratios, intrusive monitoring, and, if necessary.
Early involvement of respiratory therapy for the use of incentive spirometry or assistance with CPAP use is invaluable. Also, physical and occupational therapy for patient with restricted mobility is very useful for those who can recover functioning to ambulate. There are common immobility-related complications include skin breakdown, cardiac deconditioning, deep vein thrombosis, muscle atrophy, urinary stasis, pain management problems, constipation, and depression. Immobility also leads to pulmonary complications such as atelectasis and pneumonia.
Contraceptives
Given the increased maternal, and fetal, risk related with obesity in pregnancy, contraceptive options counseling is an essential component of preventative healthcare. Obesity can change the pharmacokinetics of medications, including contraceptives, by altering absorption, distribution and metabolism. Several studies suggest that combined hormonal contraceptives (pills/patch/ring) and progestin-only pills are less effective in women with obesity.
The U.S. Center for Disease Control and Prevention Medical Eligibility Criteria for Contraceptive Use states combined hormonal contraceptives as risk category 2 after 6 weeks postpartum in otherwise healthy women with obesity and no cardiovascular risk factors, given the low absolute risk of VTE. Women who are super-obese are not specifically addressed. Non-hormonal or progestin-only methods are safe (MEC risk category 1) immediately following delivery in all women.
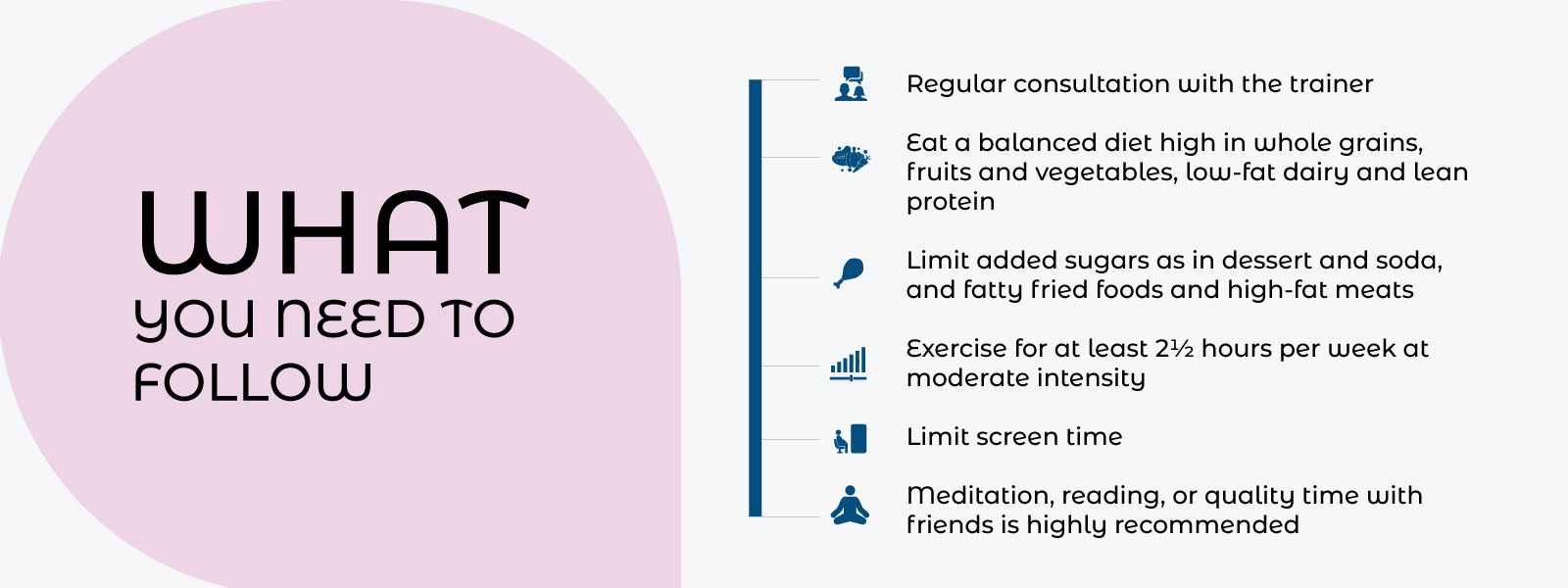
Thus, in general terms, for a person to maintain their weight balanced and follow other recommendations that are necessary, the following are the simple guidelines that one need to follow:
Key Takeaway:
The pregnancy of a patient with obesity is more complicated than the pregnancy of a normal non-obese patient with a normal BMI because the risk to the mother and the fetus increases with the level of obesity. These antepartum, intrapartum, and postpartum care needs call for more time, money, and expertise from healthcare professionals. The various health morbidities connected to obesity and super-obesity, obesity during pregnancy, have also been linked to the amplification of some of the long-term health risks. Thus, proper care and the utmost adequate facilities are required to successfully deliver the child.